- +1
快感丧失:一个被忽视的抑郁症症状

Via:《我的解放日志》
作者 | Ciara McCabe
翻译 | 卢晨曦
审校 | 酷炫脑
美工 | Jenny
编辑 | YJ
快感缺失(Anhedonia),大约75%患有抑郁症的成年人或年轻人有这种症状。尽管这一症状很常见,但它还是最难治疗和管理的症状之一。
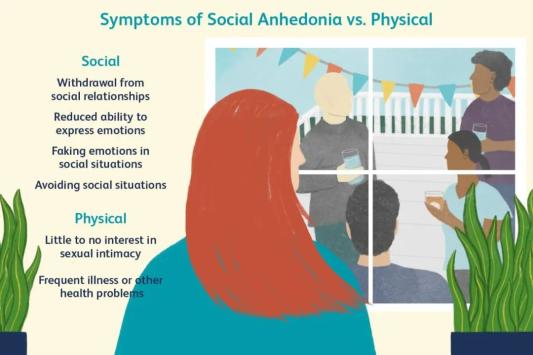
我们常常会想,如果一个人抑郁了,他们将会在大部分时间感到伤心或心情低落。但我们没有意识到的是,抑郁的症状不仅仅只有这些。另一种常被忽视的抑郁症症状则是你无法享受你以前感兴趣或喜欢的事物。
Via:verywell health
这种现象称为快感缺失(Anhedonia),大约75%患有抑郁症的成年人或年轻人有这种症状。尽管这一症状很常见,但它还是最难治疗和管理的症状之一。
丧失的快乐
快感缺失的定义是,一个人对之前他享受的活动丧失了全部的兴趣,或者减少大部分乐趣。如果一个人的快感缺失持续的时间较长(至少持续两周),即使他可能并不感到悲伤或低落,也会被诊断为抑郁症。
虽然快感缺失大部分与抑郁症有关,但它也可以是其他精神疾病的症状——比如精神分裂症、焦虑症,和帕金森。
在我和我同事对年轻人进行的有关抑郁症的深度访谈中,许多人将快感缺失不仅仅描述成失去了快乐,也把它形容成失去了做事的动力。对于一些人来说,这种动力的缺乏只与特定的事情相关——比如上学或者见朋友。但对另外一些人来说,这种情况更严重,他们觉得自己什么都不想做——甚至不想活下去。
尽管快感缺失很棘手,但它往往不是抑郁症治疗的主要目标。
我们建议,轻度抑郁症患者接受谈话治疗。中度或重度抑郁症患者可服用抗抑郁药物。虽然所有治疗方法都皆在帮助患者应对和克服症状,但半数以上的抑郁症患者对第一个推荐的治疗方法没有反应。即使更换了疗法,约30%的患者仍然会出现症状。
有人认为,对这些疗法的低反应率的原因之一可能是,目前的治疗手段并没有充分针对快感缺失。研究也表明,快感缺失可以预测抑郁症的长期复发。甚至有些抗郁郁症药物可能会加重快感缺失。

Via:giphy
为什么会这样?一种可能性是,目前标准抑郁症疗法主要治疗低落的心情,以及导致情绪低落的大脑过程,而不是快感缺失。举个例子,认知行为疗法等谈话治疗的主要目的是减少患者的消极想法。最常见的抗抑郁药物也主要针对血清素,它在一定程度上被认为是大脑处理负面信息的基础。
但正因快感缺失是对生活乐趣的减少,行为激活疗法(一种谈话治疗)对快感缺失疗效更好。这是因为行为激活疗法侧重于帮助抑郁症患者采取简单实用的措施,重新享受生活。然而,一些研究发现,行为激活疗法在控制快感缺失方面并不比标准疗法更好。这可能是因为快感缺失的本质包括动力丧失——这使得患者很难参与任何治疗,即使是对他们最有益的疗法。
快感缺失也与大脑中功能失调的奖励机制有关。因此,与目前的疗法相比,更侧重于改善大脑处理奖励的方式的治疗方法可以更有效地缓解快感缺失。
但大脑的奖励机制错综复杂,包含了各种各样的小程序——包括期待、动力、快乐、从奖励中习得经验。其中任何一种小程序出现问题,都可能导致快感缺失。因此,揭露这些小程序在快感缺失患者体内是如何运作的,就可以发现更好的治疗目标。
治疗选项
即使快感缺失很复杂,但这并不意味着为此受困的人毫无希望。
例如,研究表明,那种着重于奖励机制的谈话治疗可以缓解快感缺失。一个最近的预备试验中,被称为强化抑郁治疗(Augmented Depression Therapy)可能比行为认知疗法更好地治疗抑郁症。这是因为强化抑郁治疗专门针对快感缺失,因为病人需同时关注消极和积极的经历。
此外,针对参与奖励系统的神经递质(如多巴胺)的抗抑郁药物可能更适合快感缺失患者。对氯胺酮等可能影响多巴胺活性的药物进行的早期研究发现,氯胺酮有望治疗快感缺失。
虽然在经历快感缺失的过程中,你很难找到动力,但你仍然可试着找一些快乐的、你享受的活动,比如你曾经的爱好——或者甚至是一个新的爱好——这些都可以缓解快感缺失。
如果你认为你有快感缺失——或者其他抑郁症症状——千万不要忽视自己的感受,这样你才能得到应有的帮助和治疗。如果你不知道从何入手,可以尝试与你的亲人或医生分享你的感受。
Via:giphy
参考文献(点击滑动查看)
1. Alsayednasser, B., Widnall, E., O’Mahen, H., Wright, K., Warren, F., Ladwa, A., Khazanov, G. K., Byford, S., Kuyken, W., Watkins, E., Ekers, D., Reed, N., Fletcher, E., McMillan, D., Farrand, P., Richards, D., & Dunn, B. D. (2022). How well do Cognitive Behavioural Therapy and Behavioural Activation for depression repair anhedonia? A secondary analysis of the COBRA randomized controlled trial. Behaviour Research and Therapy, 159, 104185–104185. https://doi.org/10.1016/j.brat.2022.104185
2. Antidepressants. (2023, February 13). NHS inform. Retrieved August 23, 2023, from https://www.nhsinform.scot/tests-and-treatments/medicines-and-medical-aids/types-of-medicine/antidepressants#:%7E:text=It's%20thought%20that%20antidepressants%20work,pain%20signals%20sent%20by%20nerves.
3. Argyropoulos, S. V., & Nutt, D. J. (2013). Anhedonia revisited: is there a role for dopamine-targeting drugs for depression?. Journal of psychopharmacology (Oxford, England), 27(10), 869–877. https://doi.org/10.1177/0269881113494104
4. Behavioural Activation. (n.d). NHS Greater Manchester Mental Health. https://www.gmmh.nhs.uk/behavioural-activation/
5. Dunn, B. D. (2019). Augmenting Cognitive Behavioral Therapy to Build Positive Mood in Depression. In The Oxford Handbook of Positive Emotion and Psychopathology. Oxford University Press. https://doi.org/10.1093/oxfordhb/9780190653200.013.33
6. Dean, Z., Horndasch, S., Giannopoulos, P., & McCabe, C. (2016). Enhanced neural response to anticipation, effort and consummation of reward and aversion during bupropion treatment. Psychological Medicine, 46(11), 2263-2274. doi:10.1017/S003329171600088X
Der-Avakian, A., & Markou, A. (2012). The neurobiology of anhedonia and other reward-related deficits. Trends in Neurosciences (Regular Ed.), 35(1), 68–77. https://doi.org/10.1016/j.tins.2011.11.005
Dunn, B. D., Widnall, E., Warbrick, L., Warner, F., Reed, N., Price, A., Kock, M., Courboin, C., Stevens, R., Wright, K., Moberly, N. J., Geschwind, N., Owens, C., Spencer, A., Campbell, J., & Kuyken, W. (2023). Preliminary clinical and cost effectiveness of augmented depression therapy versus cognitive behavioural therapy for the treatment of anhedonic depression (ADepT): a single-centre, open-label, parallel-group, pilot, randomised, controlled trial. EClinicalMedicine, 61, 102084–102084. https://doi.org/10.1016/j.eclinm.2023.102084
Franken, I. H. ., Rassin, E., & Muris, P. (2007). The assessment of anhedonia in clinical and non-clinical populations: Further validation of the Snaith–Hamilton Pleasure Scale (SHAPS). Journal of Affective Disorders, 99(1), 83–89. https://doi.org/10.1016/j.jad.2006.08.020
Gorwood, P. (2008). Neurobiological mechanisms of anhedonia. Dialogues in Clinical Neuroscience, 10(3), 291–299. https://doi.org/10.31887/DCNS.2008.10.3/pgorwood
Guineau, M. G., Ikani, N., Rinck, M., Collard, R. M., van Eijndhoven, P., Tendolkar, I., Schene, A. H., Becker, E. S., & Vrijsen, J. N. (2023). Anhedonia as a transdiagnostic symptom across psychological disorders: a network approach. Psychological Medicine, 53(9), 3908–3919. https://doi.org/10.1017/S0033291722000575
Harbi, K. S. A. (2012). Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Preference and Adherence, 6(default), 369–388. https://doi.org/10.2147/PPA.S29716
Kaya, S., & McCabe, C. (2019). Can Understanding Reward Help Illuminate Anhedonia? Current Behavioral Neuroscience Reports, 6(4), 236–242. https://doi.org/10.1007/s40473-019-00186-1
Loas, G., Krystkowiak, P., & Godefroy, O. (2012). Anhedonia in Parkinson’s Disease: An Overview. The Journal of Neuropsychiatry and Clinical Neurosciences, 24(4), 444–451. https://doi.org/10.1176/appi.neuropsych.11110332
McCabe, C. (2018). Linking anhedonia symptoms with behavioural and neural reward responses in adolescent depression. Current Opinion in Behavioral Sciences, 22, 143–151. https://doi.org/10.1016/j.cobeha.2018.07.001
McCabe, C., Mishor, Z., Cowen, P. J., & Harmer, C. J. (2010). Diminished neural processing of aversive and rewarding stimuli during selective serotonin reuptake inhibitor treatment. Biological psychiatry, 67(5), 439–445. https://doi.org/10.1016/j.biopsych.2009.11.001
Moran, E. K., Culbreth, A. J., & Barch, D. M. (2022). Anhedonia in Schizophrenia. Current Topics in Behavioral Neurosciences. https://doi.org/10.1007/7854_2022_321
Nogo, D., Jasrai, A. K., Kim, H., Nasri, F., Ceban, F., Lui, L. M. W., Rosenblat, J. D., Vinberg, M., Ho, R., & McIntyre, R. S. (2022). The effect of ketamine on anhedonia: improvements in dimensions of anticipatory, consummatory, and motivation-related reward deficits. Psychopharmacology, 239(7), 2011–2039. https://doi.org/10.1007/s00213-022-06105-9
Sandman, C.F., Craske, M.G. (2022). Psychological Treatments for Anhedonia. In: Pizzagalli, D.A. (eds) Anhedonia: Preclinical, Translational, and Clinical Integration. Current Topics in Behavioral Neurosciences, vol 58. Springer, Cham. https://doi.org/10.1007/7854_2021_291
Sloat, S. (2022, January 2). Scientists untangle a link between depression and metabolism. Inverse. https://www.inverse.com/mind-body/metabolismmental-health
Spijker, J., Bijl, R. V., de Graaf, R., & Nolen, W. A. (2001). Determinants of poor 1-year outcome of DSM-III-R major depression in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Acta psychiatrica Scandinavica, 103(2), 122–130. https://doi.org/10.1034/j.1600-0447.2001.103002122.x
Treatment – depression in adults. (2023, July 5). NHS. Retrieved August 23, 2023, from https://www.nhs.uk/mental-health/conditions/depression-in-adults/treatment/
Watson, R., Harvey, K., Pass, L., McCabe, C., & Reynolds, S. (2021). A qualitative study exploring adolescents’ experience of brief behavioural activation for depression and its impact on the symptom of anhedonia. Psychology and Psychotherapy, 94(2), 266–288. https://doi.org/10.1111/papt.12307
Watson, R., Harvey, K., McCabe, C., & Reynolds, S. (2020). Understanding anhedonia: a qualitative study exploring loss of interest and pleasure in adolescent depression. European Child & Adolescent Psychiatry, 29(4), 489–499. https://doi.org/10.1007/s00787-019-01364-y
Yorbik, O., Birmaher, B., Axelson, D., Williamson, D. E., & Ryan, N. D. (2004). Clinical characteristics of depressive symptoms in children and adolescents with major depressive disorder. The Journal of Clinical Psychiatry, 65(12), 1654–1659. https://doi.org/10.4088/JCP.v65n1210


酷炫脑长期征集脑科学、心理学类文章,欢迎投稿
投稿请发邮箱:2829023503@qq.com
点这里,让朋友知道你热爱脑科学
原标题:《快感丧失:一个被忽视的抑郁症症状》
本文为澎湃号作者或机构在澎湃新闻上传并发布,仅代表该作者或机构观点,不代表澎湃新闻的观点或立场,澎湃新闻仅提供信息发布平台。申请澎湃号请用电脑访问http://renzheng.thepaper.cn。





- 报料热线: 021-962866
- 报料邮箱: news@thepaper.cn
互联网新闻信息服务许可证:31120170006
增值电信业务经营许可证:沪B2-2017116
© 2014-2024 上海东方报业有限公司